Flare Capital Partners principal Ian Chiang identifies the innovators and trends that will drive decentralization of healthcare in the coming years.
In 1751, the Pennsylvania Hospital was founded by Dr. Thomas Bond and Benjamin Franklin “to care for the sick, poor and insane who were wandering the streets of Philadelphia.” Since the founding of the so-called Nation’s First Hospital, healthcare delivery in the United States has become highly centralized over the course of two centuries.
As of today, there are 6,146 hospitals, with 924,107 total staffed beds across the U.S. (2020 AHA Hospital Statistics). In comparison, house calls by physicians all but vanished by 1980, when house calls consisted of only 0.6% of the patient-physician encounters. Like many technology and services driven industries, the healthcare delivery industry has evolved from a highly decentralized structured (community and home-based) to a centralized one (facility-based) in pursuit of operational and capital efficiency, as well as improved patient experience, by offering a one-stop-shop experience.
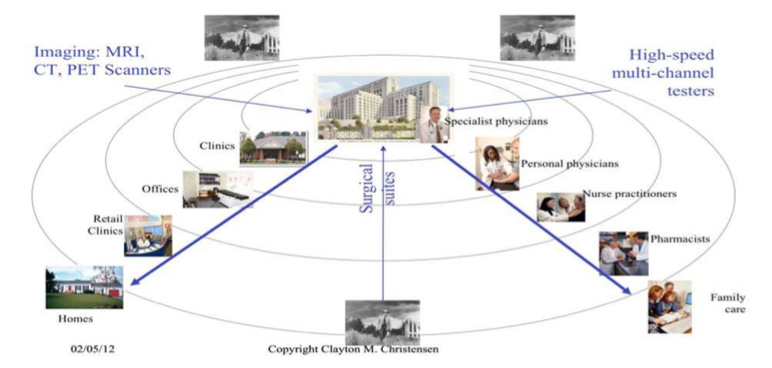
In “The Innovator’s Prescription: A Disruptive Solution for Health Care” and subsequent publications over the past decade, the late Clayton Christensen from Harvard Business School and coauthors described the onset of decentralization in healthcare that is likely to follow years of centralization. The process of decentralization (See an illustrative framework by Clayton Christensen in Figure 1) in healthcare will follow other industries (e.g., travel, retail and financial services) in which technology-enabled disruptive innovators developed ways to improve access to services (or technology) and reduce costs.
Want to publish your own articles on DistilINFO Publications?
Send us an email, we will get in touch with you.
Over the last 50 years, the industry has seen rapid decentralization of healthcare delivery services across several domains following the disruptive innovation path. Since the first Ambulatory Surgical Center opened in Phoenix, Arizona, in 1970, millions of surgeries have moved from inpatient facilities to outpatient facilities. (For example, 5,300 ASCs in the U.S. performed 23 million surgeries annually by 2011.) Many primary, preventative and urgent care services are now being delivered at retail locations (e.g., HealthHUB expansion by CVS and Walmart Health’s Health Center).
These disruptive innovations have greatly expanded access to healthcare services, and, in many cases, significantly lowered the comparative cost of care on a per procedure or per visit basis when measured against the same procedure or visit at a general hospital or a medical clinic. The rate of disruption and decentralization in healthcare delivery is accelerating as consumers, employers, health plans and governments continue to demand greater affordability and personalization in healthcare.
Most recently, the COVID-19 pandemic has profoundly changed the way healthcare services are being delivered and consumed. As patients adhere to stay-at-home and social distancing policies, facility-based visit volume has dropped precipitously. TransUnion Healthcare’s analysis of 500+ hospitals across the United States indicates a decline of 32%-60% in visit volumes between the weeks of March 1 and March 29, when compared against pre-COVID-19 volumes.
On the other hand, the U.S. has experienced a significantly increased adoption of telehealth by providers and consumers. Telehealth claim lines increased 4,347% nationally from March 2019 to March 2020, growing from .17% of medical claim lines to 7.52% over that time. There will be a day when the in-person visit volume bounces back, and the demand for virtual visits subsides. Still, the COVID-19 crisis will fundamentally change healthcare delivery and accelerate the digital health-led decentralization of healthcare delivery.
Source: Mobihealth News








